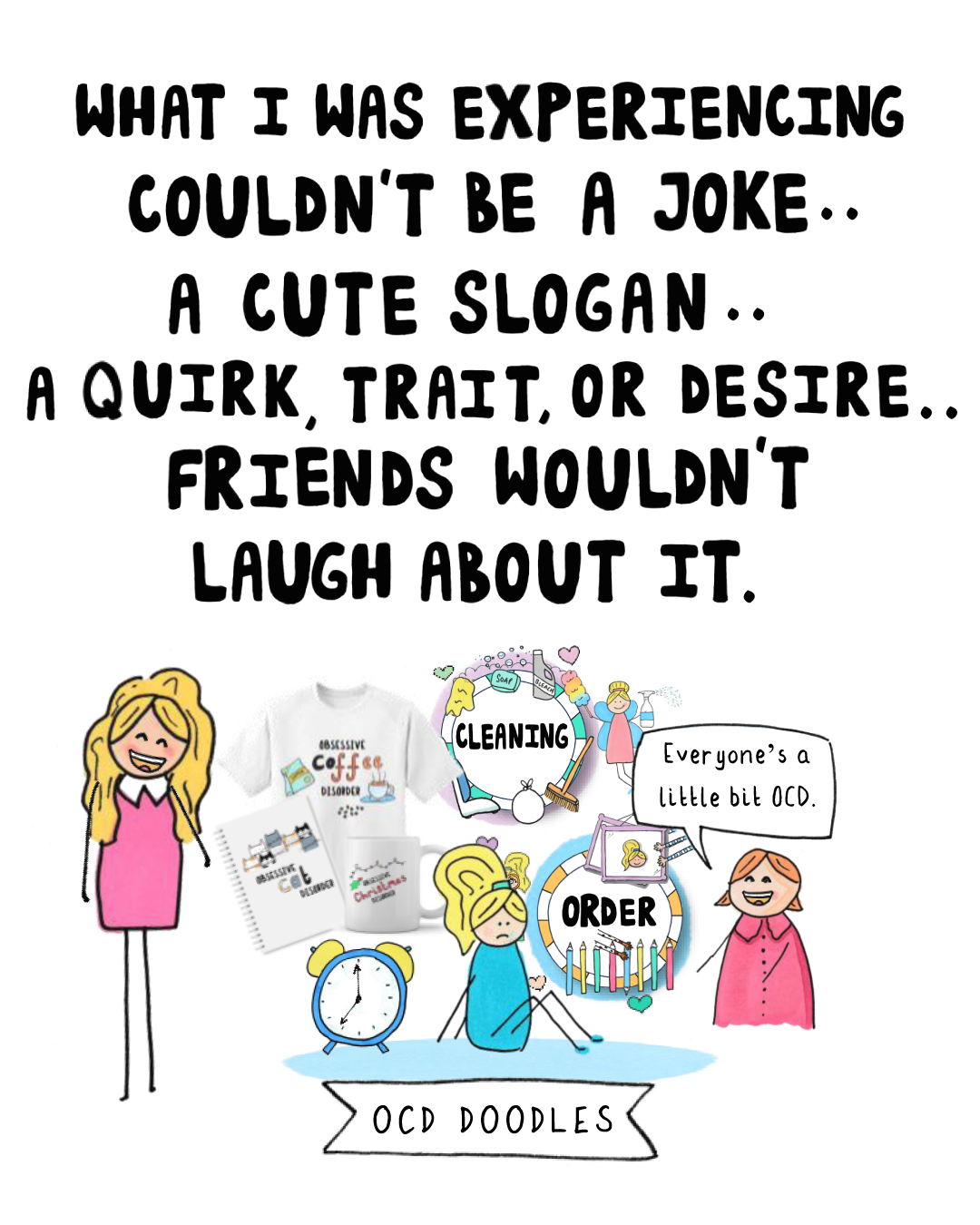
For over two decades, I believed Obsessive Compulsive Disorder (OCD) was a quirky, even desirable personality trait. I imagined it meant having a spotless room, a perfectly organized record collection (alphabetised and dusted), and a rainbow-colored wardrobe. And, I thought I’d enjoy it.
I was wrong.
The mental torment I experienced, twisting and targeting everything I loved, had nothing to do with “cute” habits. But for years, I didn’t realise it could even be OCD. Media stereotypes and casual “so OCD” jokes kept me in the dark, delaying the diagnosis and help I needed.
I want to help others avoid that delay. This page is a guide to what OCD is, how it works, and how it is treated.
OCD might not be what you think it is.
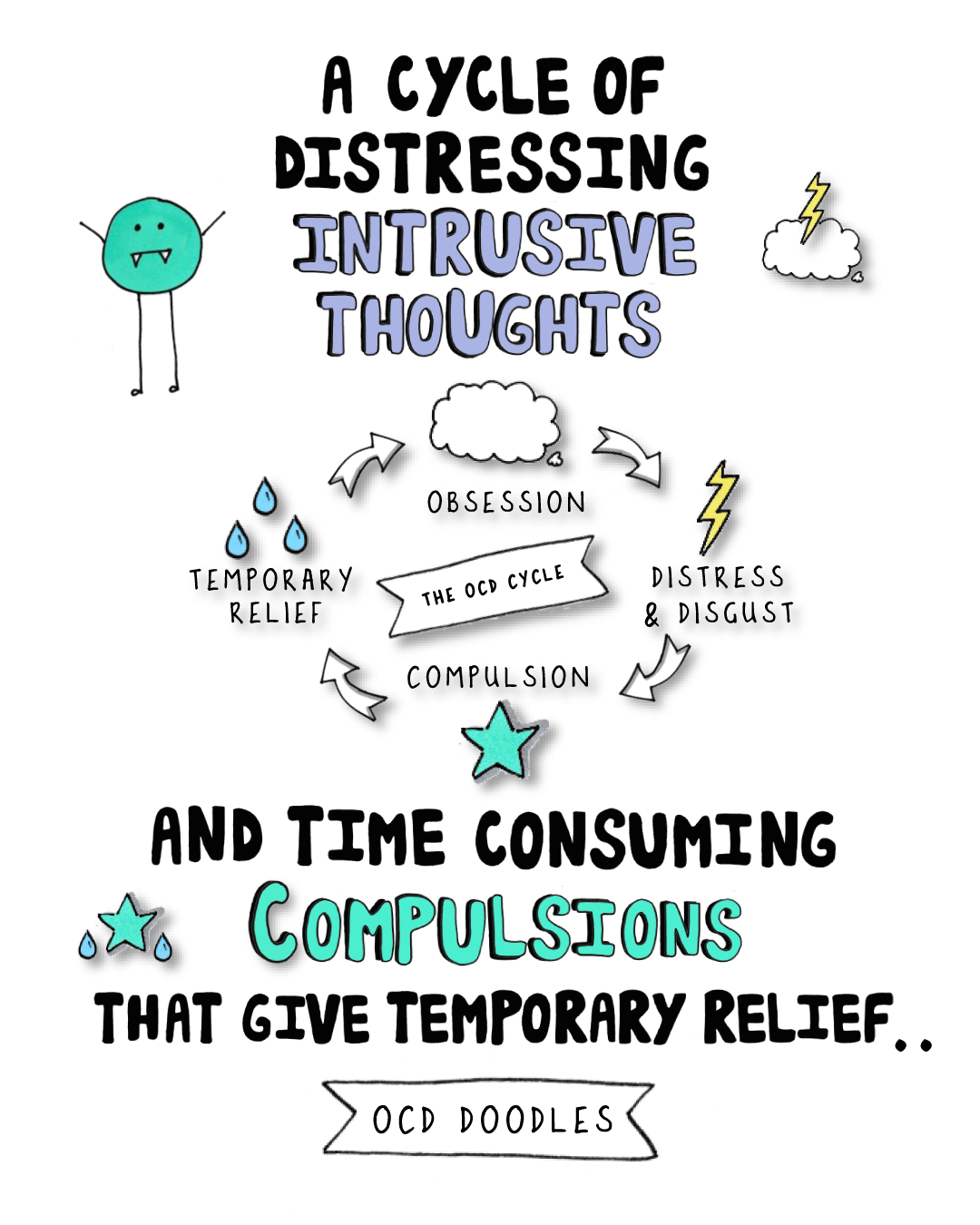
The OCD Cycle: Step by Step
OCD operates in a repetitive cycle: intrusive thoughts/obsessions → distress → compulsions → short-term relief → repeat.
Step 1: Intrusive Thoughts / Obsessions
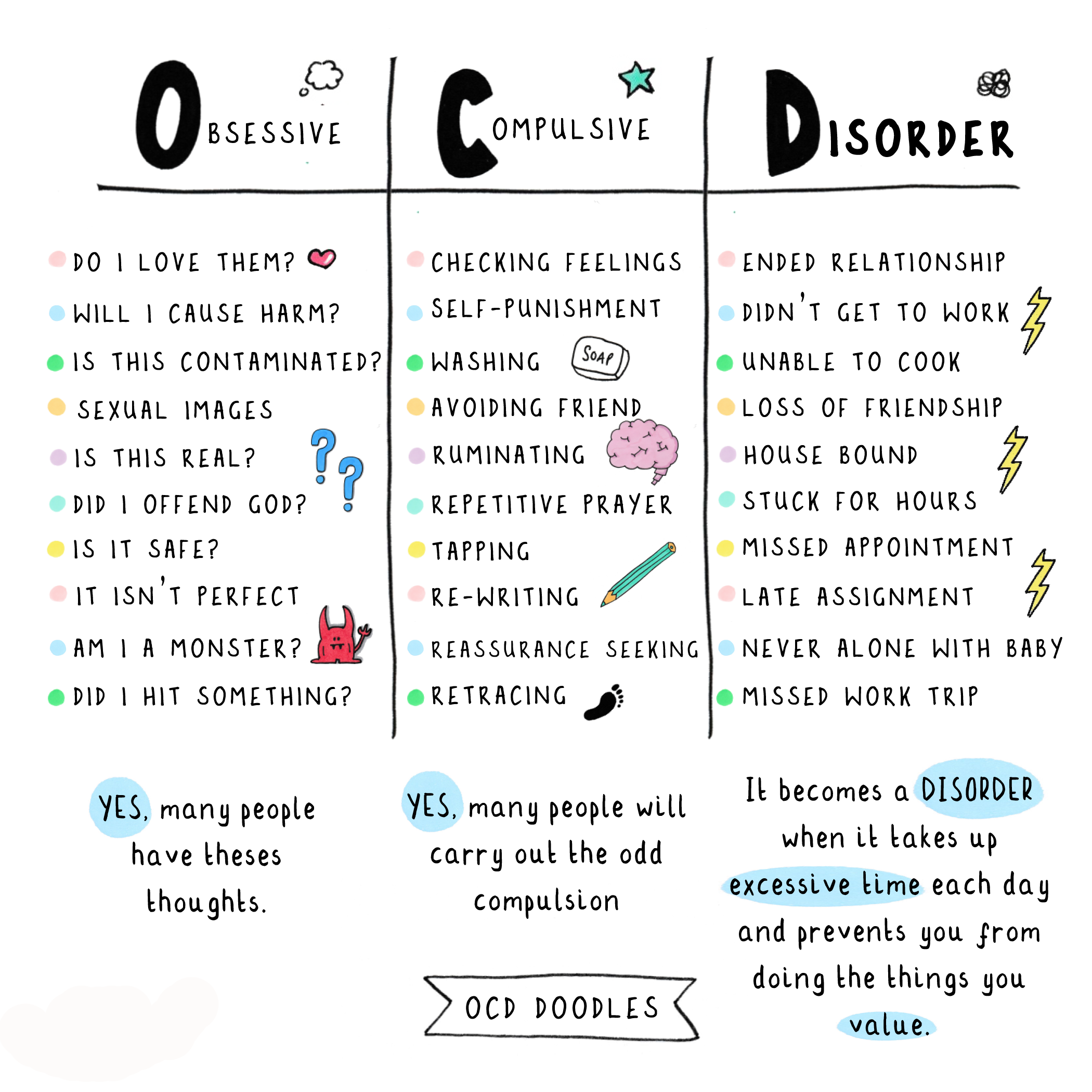
Obsessions are unwanted, repetitive thoughts or doubts. Everyone has them occasionally, but for someone with OCD, these thoughts are amplified and extremely difficult to dismiss.
Examples:
“What if I deliberately swerved my car into oncoming traffic?”
“What if I shouted an expletive in public?”
“An urge to push someone or hurt them.”
“What if someone breaks into the house and hurts my baby?”
A person without OCD might barely notice these thoughts. But with OCD, the mind attaches meaning to the thought, turning it into a distressing obsession.
Step 2: Attaching Meaning
In OCD, a thought is no longer seen as ‘just a thought’, it feels threatening, urgent, and personal:
“What does this mean about me?”
“Did I do it and can’t remember?”
“I must be a bad person.”
This step fuels the doubt spiral and makes the thought feel important, which is exhausting and overwhelming.
Step 3: Compulsions
To relieve distress, people with OCD perform compulsions -actions, mental rituals, or avoidance behaviors aimed at reducing anxiety.
Examples:
Covering your mouth in public
Neutralising intrusive thoughts with “nice” thoughts
Asking for reassurance: “Did I say anything offensive?”
Avoiding certain places altogether
Compulsions provide short-term relief, but they reinforce the OCD cycle in the long run.
Step 4: Short-Term Relief and Repetition
Compulsions relieve anxiety temporarily, teaching the brain that they “work.” When a similar intrusive thought appears again, the cycle repeats.
Common OCD Themes
OCD can appear in many forms. Some common themes include, but are not limited to:
Harm: Fears of hurting yourself or others
Relationship: Doubts about love or commitment
Sexual Orientation: Persistent doubts about sexual identity
Contamination: Fear of germs, illness, or dirt
Symmetry / Ordering: Urge for things to feel “just right”
Religious / Moral (Scrupulosity): Worries about morality or being a “bad person”
Health / Somatic: Excessive worry about illness or bodily sensations
The content of the thoughts isn’t what defines OCD but it’s the distress and compulsive response that make it a disorder.
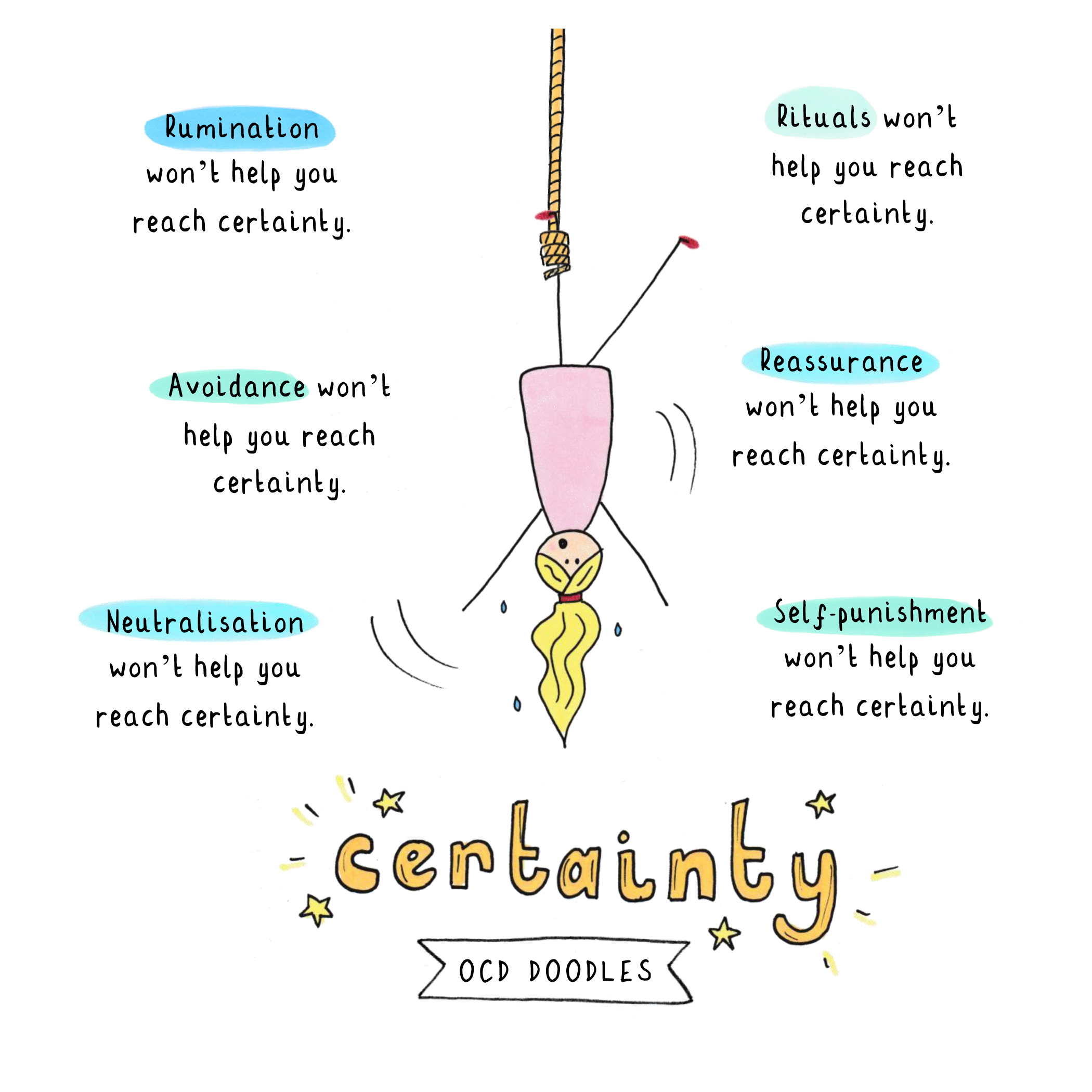
Doubt: The Heart of OCD
OCD is sometimes called “the doubting disorder” (or folie de doute in French). At its heart, it’s an intolerance of uncertainty/doubt.
Understanding this was a breakthrough for me. It simplified a disorder that had once felt all-encompassing. Instead of juggling countless “what ifs,” I could focus on one core issue: learning to tolerate doubt.
When OCD Becomes a Disorder
Obsessions and compulsions are only considered disordered when they:
Take up significant time
Cause distress
Impair daily functioning (work, relationships, socializing, self-care)
OCD is not a quirky personality trait, it’s a serious mental health condition that deserves understanding and care.
Treatment & Recovery
Exposure and Response Prevention (ERP), often combined with medication, is the NICE-recommended treatment. ERP helps break the OCD cycle by teaching people to face obsessions without performing compulsions.
Learning how ERP fits into the cycle was transformative for me. It helped me:
Understand why I was behaving the way I was
Visualise how to break the cycle
Explain my experience to loved ones
Recovery takes courage, but understanding the OCD cycle continues to help me manage OCD everday.